Credit: Judith Rudd
A new study documenting physician mistreatment during the early days of COVID-19 finds that nearly a quarter of surveyed physicians felt mistreated, harassed, or intimidated while on the job, and patients and visitors were the most frequent sources of that abuse.
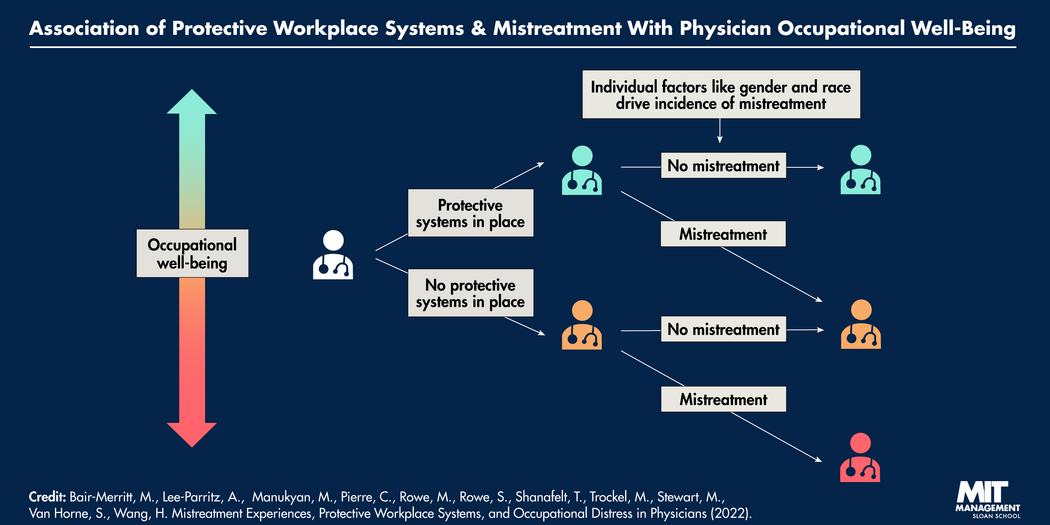
According to the paper, “Mistreatment Experiences, Protective Workplace Systems, and Occupational Distress in Physicians,” the three most common forms of mistreatment were verbal mistreatment, sexual harassment, and physical intimidation — all of which were linked to higher rates of burnout and resignations. The research also provides quantitative data showing the relationship between better occupational well-being and protective workplace systems, specifically the perception that a bystander will intervene when someone is mistreated in a workplace.
“The importance of the study is that protective measures are actually perceived to help, and that bystanders are perceived to make a difference,” said MIT Sloan adjunct professor Rowe teaches conflict management and negotiation and is currently researching bystander effectiveness.
“People care about whether their co-workers respect them enough to act on their behalf,” she said. “It’s one of the most important aspects of organizational culture.”
Rowe assisted a cohort of 10 co-researchers who surveyed 1,500 physicians at the Stanford University School of Medicine. The survey was conducted in September and October 2020. Physicians representing a variety of medical departments answered questions on whether or not they had experienced sexual harassment, verbal mistreatment, physical intimidation, or a combination of those abuses in the past 12 months, a majority of which took place during the first wave of the COVID-19 pandemic.
If a physician reported mistreatment, they were also asked the source of the mistreatment, whether there were any protective systems in their workplace, and whether bystanders spoke up in their defense.
The researchers found that any form of mistreatment was linked to a 129% greater chance of a physician having a moderate or greater intent to leave their workplace within two years. The researchers found that physicians who reported feeling there were no protective systems in place around them had a 2.41-point increase in burnout compared to physicians who felt protected. Additionally, the research showed that female and nonwhite physicians were more likely to be mistreated in some way.
Along with imbalanced gender- and race-based workplace mistreatment, abuse and harassment have real implications for hospital systems, according to the paper.
“Physician burnout threatens patient access to care through its association with increased rates of physician turnover and reduction in professional effort, which also impose additional recruitment costs on health care organizations,” the researchers write.
Mistreatment at work is linked to a 129% greater chance of a physician having a moderate or greater intent to leave their workplace within two years.
Physician burnout is also linked to more medical errors and to poorer patient care experiences and patient outcomes.
With stress and burnout already an issue in the medical field, this new finding adds an additional layer of concern around health care worker shortages. A 2021 report from the Association of American Medical Colleges predicted a shortage of primary care and non-primary care physicians by as much as 77,000 positions. And one of the main factors for that shortage is burnout.
Listening to and supporting bystanders
The survey was based on the Mistreatment, Protection, and Respect Measure, which the authors created and describe as a 7-item measure that assesses different types of mistreatment experiences, the sources of the mistreatment, and the perception of protective workplace systems.
Verbal mistreatment was the most frequent form of abuse, with 21.5% of surveyed physicians answering that they had experienced that mistreatment. Behind patients and visitors, other physicians were the second most common source of mistreatment.
The physicians were also asked whether there were good systems in place to ensure they were treated with dignity and respect, and if bystanders would speak up or intervene if someone was being mistreated. The researchers found that compared to the highest rating of bystander intervention, the lowest rating of bystander intervention was linked to a 1.08-point increase in burnout and a 1.25-point decrease in professional fulfillment.
Bystanders, according to Rowe, are people who see or learn about unacceptable behavior, but are not participating in that behavior. They notice things like abusive or inappropriate behavior, safety issues, or criminal activity. Rowe’s additional research suggests that bystanders are more likely to act and speak up about mistreatment when they feel managers are receptive to bystander actions.
Today’s leaders should support those bystanders to come forward without fear, for example, through hosting bystander training for supervisors about how to listen.
Related Articles
“The role of top leadership is powerful when leaders inform themselves in detail about what is going on in their organizations,” Rowe said.
Rowe suggested that hospitals or any organization interested in establishing protective measures and systems for bystander actions consider an integrated conflict management system.
These systems, Rowe said, “often are built on good ideas brought forward by affinity groups and work groups and [by] in-house experts working together with top leadership. The role of top leadership is powerful when leaders inform themselves in detail about what is going on in their organizations.”
The paper was published in the Journal of the American Medical Association. Rowe’s co-researchers for the paper are Dr. Susannah G. Rowe; Dr. Miriam T. Stewart; Sam Van Horne; Dr. Cassandra Pierre; Hanhan Wang; Makaila Manukyan; Dr. Megan Bair-Merritt; Dr. Aviva Lee-Parritz; Dr. Tait Shanafelt; Dr. Mickey Trockel.